Can prednisone trigger afib
Prednisone is a type of corticosteroid medication that is commonly used to treat a variety of inflammatory conditions such as arthritis, asthma, and certain types of cancer. While it is highly effective in reducing inflammation and managing symptoms, there have been concerns raised about its potential to trigger atrial fibrillation.
Atrial fibrillation is a condition characterized by an irregular and rapid heart rate. It is often associated with an increased risk of stroke, heart failure, and other cardiovascular complications. While the exact cause of atrial fibrillation is not fully understood, certain factors such as high blood pressure, heart disease, and thyroid problems can increase the risk of developing it.
Several studies have suggested that the use of corticosteroids, including prednisone, may be associated with an increased risk of atrial fibrillation. A study published in the European Heart Journal found that the use of corticosteroids was associated with a significantly higher risk of atrial fibrillation in patients with rheumatoid arthritis. Another study published in the Journal of Allergy and Clinical Immunology found that corticosteroid use was associated with an increased risk of atrial fibrillation in patients with asthma.
It is important to note that while these studies suggest a potential link between prednisone and atrial fibrillation, further research is needed to establish a definitive causal relationship. It is also important to weigh the benefits of prednisone in managing inflammatory conditions against the potential risks. If you are concerned about the potential risk of atrial fibrillation while taking prednisone, it is recommended to speak with your healthcare provider to discuss the overall risks and benefits of the medication.
What is Atrial Fibrillation?
Atrial fibrillation is a common heart rhythm disorder that affects the atria, the upper chambers of the heart. In a normal heart, the electrical signals that regulate the heartbeat originate in the sinus node, which is the heart's natural pacemaker. These signals spread across the atria and then travel to the ventricles, the lower chambers of the heart, causing them to contract and pump blood.
However, in atrial fibrillation, the electrical signals become disorganized and chaotic, causing the atria to quiver instead of contracting properly. This results in an irregular and often fast heart rate. Atrial fibrillation can have various causes, such as high blood pressure, heart disease, thyroid disorders, and excessive alcohol consumption. It can also occur as a complication of certain medical treatments or procedures.
Atrial fibrillation can lead to symptoms such as palpitations, shortness of breath, fatigue, and dizziness. It also increases the risk of more serious complications, including blood clots, stroke, and heart failure. Treatment for atrial fibrillation may involve medication to control the heart rate and rhythm, lifestyle changes, and, in some cases, procedures to restore normal heart rhythm.
Symptoms and Risk Factors
Atrial fibrillation is a medical condition that is characterized by irregular and often rapid heartbeats. Some individuals may experience symptoms such as palpitations, shortness of breath, fatigue, chest pain, and dizziness. However, it is important to note that not all people with atrial fibrillation will exhibit symptoms.
Risk factors for developing atrial fibrillation include advanced age, high blood pressure, obesity, diabetes, heart disease, smoking, excessive alcohol consumption, and a family history of the condition. Other medical factors that can increase the risk include an overactive thyroid gland, lung disease, and certain medications.
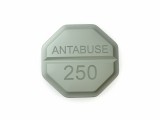
Prednisone, a type of corticosteroid medication, has been associated with an increased risk of atrial fibrillation. This medication is commonly used to treat various inflammatory conditions, such as asthma, arthritis, and allergic reactions. While prednisone can be an effective treatment, it is important to be aware of its potential side effect of triggering atrial fibrillation.
If you are prescribed prednisone and have any risk factors for atrial fibrillation, it is advised to closely monitor your heart health and report any abnormal symptoms to your healthcare provider. They may recommend additional monitoring or adjusting your medication regimen to reduce the risk of developing this condition.
Prednisone and its Effects
Prednisone is a synthetic corticosteroid that is commonly used to treat a variety of inflammatory conditions. It works by suppressing the immune system and reducing inflammation in the body. While prednisone can be an effective treatment for many conditions, it is important to be aware of its potential side effects.
Side Effects
Prednisone can cause a range of side effects, some of which can be severe. Common side effects include increased appetite, weight gain, and fluid retention. These side effects can be bothersome, but they usually resolve once the medication is stopped or the dosage is reduced.
More serious side effects of prednisone can include high blood pressure, diabetes, mood changes, and decreased bone density. Prolonged use of prednisone can also suppress the adrenal glands, which can lead to adrenal insufficiency.
Managing Side Effects
If you are taking prednisone and experiencing side effects, it is important to talk to your healthcare provider. They may be able to adjust your dosage or suggest ways to minimize the side effects. It is also important to follow a healthy lifestyle, including a well-balanced diet and regular exercise, to minimize the risk of weight gain and other complications.
Additionally, it is important to gradually taper off prednisone when discontinuing its use, as abrupt discontinuation can lead to a flare-up of symptoms and potentially adrenal insufficiency. Your healthcare provider will be able to provide guidance on the appropriate tapering schedule.
Conclusion
Prednisone can be a highly effective medication for treating a variety of conditions, but it is important to be aware of its potential side effects. By working closely with your healthcare provider and following their recommendations, you can help minimize the risks associated with prednisone while still benefitting from its therapeutic effects.
Studies on the Link between Prednisone and Atrial Fibrillation
Multiple studies have been conducted to investigate the potential link between the use of prednisone and the development of atrial fibrillation. Atrial fibrillation is a common cardiac arrhythmia characterized by irregular and rapid heartbeats, and it can lead to serious complications if left untreated.
Study 1: Retrospective Analysis
A retrospective analysis published in the Journal of Cardiology examined the medical records of patients who had taken prednisone for various medical conditions. The study found a significant association between prednisone use and the occurrence of atrial fibrillation. The researchers concluded that prednisone may indeed trigger atrial fibrillation in certain individuals.
Study 2: Randomized Controlled Trial
In a randomized controlled trial published in the European Heart Journal, researchers investigated the effect of prednisone on atrial fibrillation in patients with autoimmune diseases. The study found that those who received prednisone had a higher incidence of atrial fibrillation compared to those who received a placebo. The results suggested a potential causal relationship between prednisone and the development of atrial fibrillation.
However, it is important to note that these studies have limitations and further research is needed to fully understand the link between prednisone and atrial fibrillation. It is also worth considering that prednisone is commonly prescribed for various conditions, and atrial fibrillation may occur independently of its use.
Nevertheless, individuals who are prescribed prednisone should be monitored closely for any signs or symptoms of atrial fibrillation. If atrial fibrillation does develop, appropriate medical interventions can be implemented to address the condition and reduce the risk of complications.
Possible Mechanisms of Action
Prednisone, a type of corticosteroid medication, can potentially trigger atrial fibrillation through several mechanisms. One possible mechanism is the drug's effect on electrolyte balance. Prednisone can cause imbalances in potassium and calcium levels, which are essential for normal heart rhythm. These electrolyte imbalances can disrupt the electrical signals in the heart, leading to the development of atrial fibrillation.
Another possible mechanism is prednisone's impact on inflammation. Corticosteroids like prednisone have potent anti-inflammatory properties, which can suppress the immune response. Inflammation is a known trigger for atrial fibrillation, and by reducing inflammation, prednisone may reduce the risk of developing this arrhythmia. However, in some cases, prednisone can actually exacerbate inflammation and potentially increase the risk of atrial fibrillation.
Prednisone can also contribute to the development of atrial fibrillation by affecting the autonomic nervous system. This system controls the heart's rate and rhythm, and prednisone can disrupt its normal functioning. By altering the balance between the sympathetic and parasympathetic nervous systems, prednisone may create an environment that promotes the development of atrial fibrillation.
Additionally, prednisone can cause changes in blood pressure and heart rate, which can impact the heart's electrical activity. These changes can make the heart more susceptible to developing atrial fibrillation. It is important for individuals taking prednisone to closely monitor their heart health and report any symptoms of palpitations or irregular heartbeat to their healthcare provider.
Precautions and Recommendations
Atrial fibrillation is a serious condition, and it is important to take precautions when using prednisone or any other medication. Here are some recommendations to consider:
- Consult with your healthcare provider: It is crucial to talk to your doctor before starting any new medication, including prednisone. They can provide guidance and assess whether the benefits outweigh the risks.
- Monitor your heart rate: If you are taking prednisone and have a history of heart problems or are at a higher risk of developing atrial fibrillation, it is important to monitor your heart rate regularly. If you notice any irregularities, notify your doctor immediately.
- Follow the prescribed dosage: Prednisone should be taken exactly as prescribed by your healthcare provider. Do not exceed the recommended dosage or abruptly stop taking the medication without consulting your doctor.
- Consider alternative treatments: If you are concerned about the potential risks associated with prednisone and atrial fibrillation, discuss alternative treatment options with your healthcare provider. They may be able to recommend alternative medications or therapies that could be safer for you.
- Lead a healthy lifestyle: Maintaining a healthy lifestyle can help reduce the risk of developing atrial fibrillation. This includes regular exercise, eating a balanced diet, managing stress levels, and avoiding excessive alcohol and caffeine consumption.
Remember that every individual is unique, and the potential risk factors associated with prednisone may vary. It is essential to have an open and honest conversation with your healthcare provider to determine the best course of treatment for your specific situation.
Follow us on Twitter @Pharmaceuticals #Pharmacy
Subscribe on YouTube @PharmaceuticalsYouTube




Be the first to comment on "Can prednisone trigger afib"