Decreasing prednisone after long term use
Prednisone is a commonly prescribed corticosteroid medication that is used to treat a wide variety of medical conditions, including inflammatory diseases and autoimmune disorders. While the drug can be highly effective in managing symptoms, prolonged use of prednisone can lead to potential side effects and complications. Therefore, it is important for patients to carefully manage the gradual decrease of prednisone under the guidance of a healthcare professional.
The gradual decrease of prednisone is necessary to allow the body to adjust to the lower levels of corticosteroids. Abruptly stopping prednisone can result in adrenal insufficiency, a condition where the adrenal glands do not produce enough hormones to meet the body's needs. This can lead to symptoms such as fatigue, weakness, and low blood pressure. It is vital for patients to follow a tapering schedule that gradually reduces the dosage of prednisone over a period of time to lessen the risk of adrenal insufficiency.
When managing the gradual decrease of prednisone, healthcare professionals may prescribe a tapering schedule that takes into account the patient's individual needs and medical condition. The duration of the tapering schedule will depend on factors such as the dose of prednisone being taken, the length of time it has been taken for, and the specific condition being treated. It is important for patients to communicate any concerns or changes in symptoms to their healthcare provider, as adjustments to the tapering schedule may need to be made.
It is important to note that the gradual decrease of prednisone should always be done under medical supervision. Sudden discontinuation or improper tapering can lead to a relapse of symptoms or other adverse effects. Healthcare professionals can monitor the patient's progress, provide guidance on potential side effects, and make adjustments to the tapering schedule as needed. Patients should never attempt to decrease or discontinue prednisone without first consulting their healthcare provider.
In conclusion, proper management of the gradual decrease of prednisone is essential to minimize the potential risks and complications associated with long-term use of the medication. By following a tapering schedule under the guidance of a healthcare professional, patients can safely and effectively reduce their dosage of prednisone and transition to other treatment options if necessary. Open communication with healthcare providers is key to ensuring the best possible outcomes during the tapering process.
The Importance of Gradually Decreasing Prednisone Dosage
When it comes to managing the gradual decrease of prednisone after prolonged use, it is crucial to understand the importance of gradually decreasing the dosage. Prednisone is a corticosteroid medication that is commonly used to treat a variety of inflammatory conditions, such as asthma, allergies, and autoimmune disorders. While prednisone can be highly effective in reducing inflammation and providing relief, it is not without its potential side effects.
One of the main reasons why it is important to gradually decrease prednisone dosage is to avoid a sudden withdrawal of this medication. Abruptly stopping prednisone can lead to a range of withdrawal symptoms, including fatigue, muscle weakness, joint pain, and even adrenal insufficiency. Prednisone suppresses the production of natural cortisol in the body, and when taken for a prolonged period of time, the body becomes dependent on the medication to function properly.
By gradually tapering off prednisone, the body has time to adjust and resume its normal cortisol production. Tapering the dosage over a period of weeks or even months allows the adrenal glands to gradually reactivate and resume producing cortisol at normal levels.
Additionally, a gradual decrease in prednisone dosage helps to minimize the risk of flare-ups or worsening of the underlying condition. Prednisone is often prescribed to manage symptoms of various inflammatory conditions, and a sudden reduction in dosage can trigger a rebound effect, causing a resurgence of symptoms.
Furthermore, tapering off prednisone can help to identify the lowest effective dosage for long-term management of the condition. By slowly reducing the dosage, healthcare professionals can closely monitor the patient's response and adjust the medication accordingly. This approach reduces the risk of overmedication and allows for a more individualized treatment plan.
In conclusion, gradually decreasing prednisone dosage is essential for a smooth transition off this medication after prolonged use. By doing so, patients can avoid withdrawal symptoms, allow their bodies to regain normal cortisol production, minimize the risk of flare-ups, and identify the optimal long-term dosage for managing their condition effectively.
Understanding Prednisone Therapy
What is Prednisone?
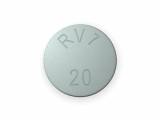
Prednisone is a synthetic corticosteroid medication that is commonly prescribed to treat a variety of conditions, such as inflammation, allergies, and autoimmune disorders. It belongs to a class of drugs known as glucocorticoids, which mimic the effects of cortisol, a hormone produced by the adrenal glands.
How Does Prednisone Work?
Prednisone works by suppressing the immune system and reducing inflammation in the body. It does this by inhibiting the production of certain chemicals that play a role in the immune response. This helps to alleviate symptoms such as pain, swelling, redness, and itching.
Benefits of Prednisone Therapy
Prednisone therapy can provide relief from a wide range of symptoms associated with inflammatory and immune-related conditions. It can help to reduce pain and swelling, improve breathing, control allergic reactions, and manage autoimmune disorders. Additionally, prednisone can be used as a bridge therapy while waiting for other long-term treatments to take effect.
Potential Side Effects
While prednisone can be an effective treatment option, it is important to be aware of its potential side effects. Some common side effects of prednisone include increased appetite, weight gain, mood changes, difficulty sleeping, and fluid retention. Long-term use of prednisone can also lead to more serious side effects, such as osteoporosis, diabetes, and adrenal insufficiency.
Managing Prednisone Therapy
When prescribed prednisone therapy, it is important to follow the dosage instructions provided by your healthcare provider. Abruptly stopping prednisone can cause withdrawal symptoms, so it is typically tapered off gradually to allow the body to adjust. Your healthcare provider may also recommend lifestyle modifications, such as a healthy diet, regular exercise, and calcium and vitamin D supplementation, to help minimize the risk of side effects.
Conclusion
Prednisone therapy can be a valuable treatment option for various inflammatory and immune-related conditions. Understanding how prednisone works, its potential benefits and side effects, and how to effectively manage the therapy can help ensure its safe and effective use.
Potential Side Effects of Prolonged Prednisone Use
1. Adrenal Suppression:
Prolonged use of prednisone can suppress the function of the adrenal glands, which are responsible for producing natural steroid hormones in the body. This can lead to adrenal insufficiency, where the body is unable to produce enough cortisol on its own. Symptoms of adrenal suppression may include fatigue, weakness, low blood pressure, and electrolyte imbalances.
2. Osteoporosis:
Prednisone can cause bone loss and increase the risk of osteoporosis, a condition characterized by weakened and brittle bones. Prolonged use of prednisone can lead to a decrease in bone density due to its effect on calcium absorption and bone remodeling. It is important to take measures to prevent osteoporosis, such as getting adequate calcium and vitamin D, engaging in weight-bearing exercises, and, if necessary, taking medications to improve bone strength.
3. Weight Gain:
Prednisone can cause fluid retention and increased appetite, leading to weight gain. This can be particularly problematic when the medication is used for a long period of time. Managing calorie intake and participating in regular physical activity can help mitigate this side effect.
4. Mood Changes:
Prolonged use of prednisone can affect mood and behavior. Some individuals may experience irritability, anxiety, or depression while taking the medication. It is important to monitor and communicate any changes in mood to a healthcare professional, as they may need to adjust the dosage or prescribe additional medications to manage these symptoms.
5. Infection Risk:
Prednisone suppresses the immune system, making individuals more susceptible to infections. Prolonged use of the medication can increase the risk of developing infections and may also impair the body's ability to fight off infections. It is important to take precautions to minimize the risk of infection, such as practicing good hygiene, avoiding contact with sick individuals, and getting vaccinated as recommended.
6. Eye Problems:
Prednisone use can cause various eye-related side effects, including cataracts and glaucoma. Prolonged use of the medication may increase the risk of developing these conditions. Regular eye exams and monitoring by an ophthalmologist are essential to detect and manage any eye problems associated with prednisone use.
7. Avascular Necrosis:
Prednisone use has been associated with avascular necrosis, a condition characterized by the death of bone tissue due to a lack of blood supply. Prolonged use of the medication can increase the risk of developing avascular necrosis, particularly in the hip joints. Close monitoring and early detection of this condition are important to prevent further damage and provide appropriate treatment.
Overall, while prednisone can be an effective medication for managing various conditions, prolonged use can lead to a range of potential side effects. It is important for individuals taking prednisone to be aware of these risks and work closely with their healthcare provider to minimize them and find the most appropriate treatment plan.
Managing the Tapering Process
Tapering off prednisone after prolonged use requires careful management to minimize potential side effects and ensure a smooth transition. Here are some key steps to help manage the tapering process:
1. Consultation with a Healthcare Provider
Before starting the tapering process, it is important to consult with a healthcare provider who can evaluate your individual situation and provide specific guidance. They will consider factors such as the length of prednisone use, the dosage, and the underlying condition for which prednisone was prescribed.
2. Gradual Reduction of Dosage
The tapering process involves gradually reducing the dosage of prednisone over a predetermined period of time. This allows the body to adjust to lower levels of the medication and helps minimize withdrawal symptoms. The specific tapering schedule will depend on the individual's condition and response to the medication.
3. Monitoring for Side Effects
During the tapering process, it is important to closely monitor for any potential side effects. These may include symptoms such as fatigue, muscle weakness, mood changes, or increased pain. If any new or worsening symptoms occur, it is important to contact your healthcare provider for further evaluation.
4. Supportive Measures
Supportive measures can play a role in managing the tapering process. These may include incorporating a healthy lifestyle, such as regular exercise, a balanced diet, and stress management techniques. Supportive therapies, such as physical therapy or acupuncture, may also be beneficial in managing symptoms during the tapering process.
5. Regular Follow-up with Healthcare Provider
Regular follow-up appointments with a healthcare provider are essential throughout the tapering process. This allows for monitoring of the individual's progress, evaluation of any side effects, and adjustment of the tapering schedule if needed. Open communication with the healthcare provider is crucial to ensure the tapering process is going smoothly.
In conclusion, managing the tapering process after prolonged use of prednisone requires a thoughtful and individualized approach. By following these steps and working closely with a healthcare provider, the transition off prednisone can be successfully managed, minimizing side effects and promoting overall well-being.
Advice for Patients During Prednisone Tapering
1. Follow your doctor's instructions
It is important to strictly adhere to the tapering schedule provided by your doctor. This schedule is tailored to your specific condition and is designed to minimize withdrawal symptoms and potential complications.
2. Monitor your symptoms
Pay close attention to how you are feeling during the prednisone tapering process. Report any changes or worsening of symptoms to your doctor. This will help them adjust the tapering schedule if necessary and ensure your safety and well-being.
3. Take it slow
A gradual decrease in prednisone dosage is often recommended to allow your body to adjust and minimize the risk of adrenal insufficiency. Stick to the prescribed tapering schedule and avoid rushing the process, even if you start feeling better.
4. Maintain a healthy lifestyle
During the prednisone tapering period, it is important to support your body's natural healing processes. This includes eating a balanced diet, getting regular exercise, and getting enough rest. Avoid excessive stress and take care of your mental health as well.
5. Keep an eye on potential side effects
As you taper off prednisone, watch out for any side effects that may arise. These can include mood swings, increased appetite, weight gain, insomnia, or changes in the appearance of your skin. Report any concerns to your doctor.
6. Communicate with your healthcare team
Openly communicate with your doctor and other healthcare providers involved in your care. They can provide guidance and address any concerns you may have during the prednisone tapering process. Regular check-ups and follow-up appointments are important for monitoring your progress.
Monitoring and Support from Healthcare Professionals
To ensure a safe and successful tapering process of prednisone, it is important to have ongoing monitoring and support from healthcare professionals. Regular check-ups with a healthcare provider are essential to assess the progress of tapering and to make any necessary adjustments to the dosage. These check-ups may include physical examinations, blood tests, and discussions about any new or worsening symptoms.
In addition to regular check-ups, healthcare professionals can provide guidance and support throughout the tapering process. They can help individuals understand the potential side effects of prednisone withdrawal and how to manage them. They may also recommend lifestyle modifications, such as changes in diet and exercise, to support the body during the transition period.
Healthcare professionals can also assist in developing a personalized tapering plan based on individual needs and medical history. They can determine the appropriate duration for tapering, the rate at which to decrease the dosage, and any additional medications that may be needed to manage symptoms or underlying conditions. This individualized approach helps to minimize the risk of relapse or rebound symptoms during the tapering process.
Furthermore, healthcare professionals can provide emotional support and address any concerns or fears that individuals may have about tapering off prednisone. They can help individuals navigate any challenges or difficulties that arise during the process and provide reassurance that tapering is a normal and necessary part of treatment for prolonged prednisone use.
Long-Term Strategies for Maintaining Health and Well-Being
When it comes to maintaining health and well-being in the long-term, there are several strategies that can be helpful. One important aspect is maintaining a balanced and nutritious diet. Including a variety of fruits, vegetables, whole grains, lean proteins, and healthy fats can provide the body with the essential nutrients it needs to function properly. Additionally, staying hydrated by drinking an adequate amount of water each day is crucial for overall health.
An active lifestyle is another key factor in maintaining health and well-being. Engaging in regular exercise can help improve cardiovascular health, increase strength and flexibility, and boost mood. Finding activities that are enjoyable and can be sustained long-term is important to maintain motivation and consistency. This could include activities such as walking, cycling, swimming, or participating in group fitness classes.
Furthermore, managing stress levels is essential for overall health and well-being. Chronic stress can have a negative impact on both physical and mental health. Engaging in stress-reducing practices such as meditation, deep breathing exercises, or yoga can help to promote relaxation and reduce stress levels. Additionally, prioritizing self-care activities, such as taking time for hobbies, spending time in nature, or practicing mindfulness, can also contribute to overall well-being.
In addition to these strategies, it is important to prioritize regular visits to healthcare professionals. This includes scheduling routine check-ups, screenings, and vaccinations to ensure any potential health issues are identified and addressed in a timely manner. Building a strong relationship with a primary care physician can provide guidance and support in maintaining health and well-being in the long-term.
Overall, maintaining health and well-being in the long-term requires a multifaceted approach that includes a balanced diet, regular exercise, stress management, and regular healthcare visits. By adopting these strategies and making them a consistent part of daily life, individuals can enhance their overall quality of life and reduce the risk of developing chronic diseases or other health conditions.
Follow us on Twitter @Pharmaceuticals #Pharmacy
Subscribe on YouTube @PharmaceuticalsYouTube




Be the first to comment on "Decreasing prednisone after long term use"