Nursing consideration for prednisone
Prednisone is a corticosteroid medication commonly used to treat a variety of conditions such as asthma, allergies, and autoimmune disorders. As a nurse administering prednisone, it is important to have a thorough understanding of the medication, its indications, and potential side effects.
One important nursing consideration for prednisone administration is to closely monitor the patient for adverse reactions. Prednisone can cause a range of side effects, including increased appetite, weight gain, fluid retention, and mood changes. It is crucial to assess the patient regularly for any changes in their physical and emotional well-being.
The dosage and administration of prednisone also require careful attention. The medication is usually prescribed as a tapering dose, starting with a higher dose and gradually reducing over time. Nurses should ensure that the patient understands the dosing schedule and follows it accordingly. It is important to educate the patient about the importance of not abruptly stopping prednisone, as sudden withdrawal can lead to adrenal insufficiency.
Furthermore, nurses should be aware of potential drug interactions with prednisone. Prednisone can interact with certain medications, such as anticoagulants and nonsteroidal anti-inflammatory drugs (NSAIDs), increasing the risk of bleeding. Nurses should review the patient's medication list and communicate with the healthcare team if any potential interactions are identified.
In summary, nursing considerations for prednisone administration involve monitoring for adverse reactions, ensuring proper dosage and administration, and being aware of potential drug interactions. By being diligent in these considerations, nurses can help promote the safe and effective use of prednisone in their patients.
Patient Assessment for Prednisone Administration
Prednisone is a corticosteroid medication that is commonly prescribed for a variety of medical conditions. Before administering prednisone to a patient, it is important to conduct a thorough patient assessment to ensure safe and effective administration of the medication.
Medical history: Obtain a detailed medical history from the patient, including any previous or current medical conditions, allergies, and medications. Prednisone may interact with certain medications and exacerbate certain medical conditions, so it is essential to gather this information.
Physical examination: Perform a comprehensive physical examination to assess the patient's overall health status. Focus on assessing vital signs, respiratory function, and any specific areas of concern related to the patient's medical condition. Document any abnormalities or concerns that may impact the safe administration of prednisone.
Laboratory tests: Order relevant laboratory tests to assess the patient's baseline values and determine if any adjustments or precautions are necessary before administering prednisone. This may include blood tests, such as complete blood count, liver function tests, and kidney function tests.
Patient education: Provide the patient with information about prednisone, its potential side effects, and the importance of adhering to the prescribed dosage and schedule. Discuss any specific considerations or precautions related to the patient's medical condition and provide written educational materials, if available.
Monitoring: Plan for ongoing monitoring of the patient's response to prednisone. This may include regular assessments of vital signs, blood glucose levels (especially for patients with diabetes), and any specific parameters related to the patient's medical condition. Adjustments to the dosage or schedule may be needed based on the patient's individual response.
Collaboration: Communicate and collaborate with other healthcare providers involved in the patient's care, such as physicians, pharmacists, and other members of the healthcare team. Share the findings from the patient assessment and work together to develop a comprehensive plan for prednisone administration.
By conducting a thorough patient assessment and implementing appropriate monitoring and education, healthcare professionals can ensure safe and effective administration of prednisone to patients. This assessment helps identify any potential complications or interactions that may arise during treatment, allowing for proactive management and improved patient outcomes.
Monitoring and Managing Prednisone Side Effects
When administering prednisone to patients, it is important for nurses to closely monitor and manage the potential side effects that may arise. Prednisone is a corticosteroid medication used to treat various conditions, but it can also cause a range of adverse effects that can impact patient well-being.
Close monitoring of vital signs
One important aspect of monitoring prednisone side effects is closely monitoring the patient's vital signs. This includes regularly checking their blood pressure, heart rate, temperature, and oxygen saturation. Prednisone can increase blood pressure and heart rate, so it is crucial to ensure these values are within an acceptable range.
Assessment of fluid and electrolyte imbalance
Prednisone can lead to fluid retention and electrolyte imbalances, such as sodium and potassium disturbances. Nurses must assess for signs of fluid overload or dehydration and monitor the patient's electrolyte levels through laboratory tests. This can help identify any imbalances early and allow for appropriate interventions.
Managing gastrointestinal side effects
Gastrointestinal side effects are common with prednisone use, including stomach ulcers, nausea, and increased appetite. Nurses can provide education on dietary modifications to mitigate these effects, such as avoiding spicy or acidic foods and eating smaller, more frequent meals. Medications to protect the stomach lining, such as proton pump inhibitors or H2 blockers, may also be prescribed.
Prevention and treatment of osteoporosis
Prednisone can cause bone loss and increase the risk of osteoporosis in long-term users. Nurses can promote bone health by encouraging weight-bearing exercises, ensuring an adequate intake of calcium and vitamin D, and discussing the potential need for a bone density scan or osteoporosis medications.
Regular glucose monitoring
Prednisone can lead to elevated blood glucose levels, especially in individuals with pre-existing diabetes or prediabetes. Nurses should monitor their patient's blood glucose levels regularly and educate them on the signs and symptoms of hyperglycemia. It may be necessary to adjust insulin or oral antidiabetic medication dosages to maintain glycemic control.
Dosage and Administration of Prednisone
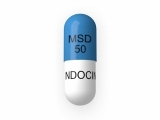
Prednisone is a corticosteroid medication commonly prescribed for various medical conditions. The dosage of prednisone is determined by the healthcare provider and varies depending on the condition being treated, the severity of symptoms, and the individual patient's response to the medication.
Oral Administration: Prednisone is most commonly administered orally in tablet or liquid form. The healthcare provider will prescribe a specific dosage and provide instructions on when and how to take the medication.
Dosage: The dosage of prednisone can range from a low dose, such as 5 to 10 milligrams per day, to a high dose, such as 60 to 80 milligrams per day. The dosage may be tapered up or down depending on the patient's response to the medication and the healthcare provider's recommendations.
Dosage Regimen: In some cases, the healthcare provider may prescribe a single daily dose of prednisone, while in other cases, the dosage may be split into multiple smaller doses throughout the day. The dosage regimen will depend on the specific needs of the patient and the condition being treated.
Monitoring and Adjustments: It is important for healthcare providers to closely monitor patients receiving prednisone and adjust the dosage as needed. This may involve regular check-ups, blood tests, and evaluation of the patient's symptoms and overall health.
Special Considerations: Certain factors may affect the dosage and administration of prednisone, such as the patient's age, weight, underlying medical conditions, and concomitant use of other medications. It is important for healthcare providers to consider these factors when prescribing prednisone and to closely monitor the patient for any potential side effects or interactions.
Drug Interactions with Prednisone
Prednisone is a powerful corticosteroid commonly used to treat a variety of medical conditions. It is important for nurses to be aware of potential drug interactions with prednisone to ensure safe and effective patient care.
Interactions with OTC medications:
Prednisone can interact with over-the-counter (OTC) medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs) and aspirin. These medications may increase the risk of gastrointestinal bleeding or stomach ulcers when taken together with prednisone. Nurses should monitor patients for signs of gastrointestinal bleeding, such as abdominal pain or black, tarry stools.
Interactions with other prescription medications:
Prednisone can interact with other prescription medications, including anticoagulants (blood thinners) and antidiabetic drugs. When taken with prednisone, anticoagulants may increase the risk of bleeding, while antidiabetic drugs may increase blood sugar levels. Nurses should monitor patients' INR levels if they are taking both prednisone and anticoagulants, and closely monitor blood glucose levels if patients are taking antidiabetic drugs.
Interactions with herbal supplements:
Herbal supplements, such as St. John's wort and echinacea, can interact with prednisone and reduce its effectiveness. Nurses should educate patients about potential interactions between herbal supplements and prednisone, and advise patients to consult their healthcare provider before taking any new supplements.
Interactions with vaccines:
Prednisone can affect the body's response to vaccines, reducing their effectiveness. Nurses should inquire about a patient's vaccination history before administering vaccines, and consult with the healthcare provider if the patient is currently taking prednisone.
In conclusion, nurses should be aware of potential drug interactions with prednisone to ensure safe and effective patient care. This includes monitoring for gastrointestinal bleeding when taken with NSAIDs or aspirin, monitoring INR levels when taken with anticoagulants, monitoring blood glucose levels when taken with antidiabetic drugs, educating patients about interactions with herbal supplements, and considering the impact on vaccines. By being knowledgeable about these interactions, nurses can provide optimal care to patients receiving prednisone therapy.
Patient Education and Counseling for Prednisone
Patient education and counseling are crucial components of prednisone administration. It is essential for healthcare providers to provide comprehensive information to patients to ensure safe and effective use of the medication.
Key Points for Patient Education
1. Proper Dosage: Patients should understand the importance of taking prednisone as prescribed by their healthcare provider. They should be educated about the specific dosage, duration of treatment, and frequency of administration. It is important to emphasize the need to strictly follow the prescribed regimen to achieve the intended therapeutic effects.
2. Potential Side Effects: Patients should be informed about the possible side effects of prednisone. Common side effects may include weight gain, fluid retention, mood changes, insomnia, and increased appetite. It is important to explain that these side effects are usually temporary and will subside once the medication is discontinued. However, severe or persistent side effects should be reported to the healthcare provider.
3. Adverse Reactions: Patients should be educated about the signs of potential adverse reactions, such as allergic reactions, infection, or gastrointestinal bleeding. They should be instructed to seek immediate medical attention if they experience symptoms such as difficulty breathing, severe rash, fever, or prolonged bleeding.
4. Medication Interactions: Patients should be counseled on potential drug interactions with prednisone. They should be advised to inform their healthcare provider about all the medications, supplements, and herbal products they are taking to avoid any potential interactions.
Lifestyle Recommendations for Patients Taking Prednisone
1. Diet: Patients should be advised to follow a healthy and balanced diet while taking prednisone. They should be encouraged to limit their intake of sodium, sugar, and processed foods to help manage weight gain and fluid retention.
2. Exercise: Patients should be encouraged to engage in regular exercise, as it can help alleviate some of the common side effects of prednisone, such as weight gain and mood changes. However, they should consult with their healthcare provider before starting any new exercise routine.
3. Stress Management: Patients should be counseled on stress management techniques, as prednisone can sometimes exacerbate stress-related symptoms. They should be advised to practice relaxation techniques, such as deep breathing exercises and mindfulness, to help cope with stress.
4. Regular Check-ups: Patients should be informed about the importance of regular check-ups and monitoring while taking prednisone. They should be encouraged to schedule follow-up appointments with their healthcare provider to ensure the medication's effectiveness and monitor any potential side effects or adverse reactions.
By providing comprehensive patient education and counseling, healthcare providers can help patients navigate the use of prednisone and optimize treatment outcomes while minimizing potential risks.
Follow-up and Evaluation of Prednisone Therapy
Monitoring for Side Effects
After initiating prednisone therapy, it is important for healthcare providers to closely monitor patients for any potential side effects. Common side effects of prednisone include increased appetite, weight gain, fluid retention, mood changes, difficulty sleeping, and gastrointestinal disturbances. Severe side effects, such as adrenal insufficiency, hyperglycemia, and osteoporosis, may also occur with prolonged use of prednisone. Regular assessments, including physical examinations, laboratory tests, and patient interviews, should be conducted to detect and manage any adverse reactions that may be correlated with prednisone therapy.
Assessing Treatment Response
To evaluate the effectiveness of prednisone therapy, healthcare providers should monitor patients for improvement in their symptoms or underlying conditions. For example, if prednisone is being used to treat an inflammatory condition, such as rheumatoid arthritis or asthma, the patient's pain levels, joint mobility, and lung function should be assessed periodically. It is important to note that response to prednisone can vary among individuals, so a tailored approach is necessary. Adjustments in dosage or the addition of other treatments may be needed to achieve optimal outcomes.
Education and Counseling
During follow-up visits, healthcare providers should take the opportunity to provide patients with education and counseling regarding prednisone therapy. This may include explaining the purpose of the medication, its potential side effects, and any lifestyle modifications that may be necessary. Patients should be encouraged to ask questions and voice any concerns they may have. Emphasizing adherence to the prescribed dosage and schedule is crucial for maximizing the benefits of prednisone therapy while minimizing potential risks. Additionally, patients should be informed about symptoms that require immediate medical attention, such as severe allergic reactions or signs of adrenal suppression.
Collaboration and Referral
Follow-up and evaluation of prednisone therapy may also involve collaboration with other healthcare providers. For example, if a patient develops complications or requires specialized care, a referral to a rheumatologist, pulmonologist, or endocrinologist may be necessary. Ongoing communication between the patient's primary care provider and any specialist involved is essential for ensuring comprehensive and coordinated care. Collaborative efforts can help optimize the management of prednisone therapy and address any challenges or concerns that may arise during the course of treatment.
Follow us on Twitter @Pharmaceuticals #Pharmacy
Subscribe on YouTube @PharmaceuticalsYouTube




Be the first to comment on "Nursing consideration for prednisone"