Prednisone cause afib
Prednisone is a medication that is commonly prescribed for a variety of conditions, including autoimmune diseases, asthma, and allergies. While it is an effective treatment for many patients, there have been reports of prednisone causing or exacerbating atrial fibrillation, a type of irregular heartbeat.
Atrial fibrillation, also known as AFib, is a condition in which the heart's normal rhythm is disrupted, causing the upper chambers of the heart to quiver instead of contracting normally. This can lead to a variety of symptoms, including palpitations, shortness of breath, and fatigue.
Research is still ongoing to understand the relationship between prednisone and atrial fibrillation. Some studies have found an increased risk of AFib in patients taking prednisone, while others have not found a significant association. It is important to note that AFib can also be caused by other factors, such as age, high blood pressure, and heart disease.
If you are taking prednisone and experiencing symptoms of atrial fibrillation, it is important to speak with your healthcare provider. They can evaluate your condition and determine the best course of action. They may recommend adjusting your medication dosage, or exploring other treatment options to manage your symptoms.
It is always important to weigh the benefits of any medication against the potential risks, and this is especially true for prednisone. While it can be an effective treatment for many conditions, including autoimmune diseases, it is important to be aware of the potential side effects, such as atrial fibrillation. Your healthcare provider can help you make an informed decision about your treatment options.
What Is Atrial Fibrillation?
Atrial fibrillation (AF) is a common heart rhythm disorder that affects the upper chambers of the heart, known as the atria. Normally, the atria contract in a coordinated manner to pump blood into the lower chambers of the heart (ventricles) and out to the rest of the body. However, in AF, the electrical signals that control the heartbeat become disorganized, causing the atria to quiver or fibrillate instead of contracting effectively.
AF can cause a variety of symptoms, including palpitations, rapid or irregular heartbeat, fatigue, shortness of breath, dizziness, and fainting. It can also increase the risk of blood clots forming in the heart, which can then travel to other parts of the body and cause serious complications, such as stroke.
There are several different types of AF, including paroxysmal AF (episodes that come and go), persistent AF (longer episodes that require treatment to restore normal rhythm), and permanent AF (continuous AF that cannot be restored to normal rhythm).
The exact cause of AF is often unknown, but it is believed to be related to various factors, including age, high blood pressure, heart disease, thyroid problems, obesity, excessive alcohol or caffeine consumption, and certain medications.
Diagnosis of AF typically involves an electrocardiogram (ECG) to assess the heart's electrical activity, along with a physical examination and medical history review. Treatment options include medication to control the heart rate and rhythm, blood thinners to prevent clot formation, and procedures to restore normal rhythm, such as cardioversion or catheter ablation.
Understanding Prednisone
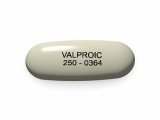
Prednisone is a medication that belongs to a class of drugs known as corticosteroids. It is commonly used to treat conditions such as severe allergies, asthma, rheumatoid arthritis, and certain autoimmune disorders. Prednisone works by suppressing the immune system and reducing inflammation in the body.
Usage: Prednisone is usually taken orally in the form of tablets or liquid, and the dosage and duration of treatment are determined by the healthcare provider based on the specific condition being treated. It is important to follow the prescribed dosage and schedule as abruptly stopping the medication can cause withdrawal symptoms.
Side Effects:
Prednisone can cause a range of side effects, some of which may be more severe than others. Common side effects include increased appetite, weight gain, mood changes, insomnia, and fluid retention. Long-term use of prednisone can also lead to more serious side effects such as osteoporosis, diabetes, and adrenal insufficiency.
Risks vs Benefits: While prednisone can be highly effective in treating certain conditions, it is essential to weigh the potential risks against the benefits. The medication should only be used when the potential benefits outweigh the risks, and the healthcare provider will carefully monitor the patient's response to the treatment to ensure its safety and effectiveness.
Drug Interactions:
Prednisone can interact with other medications, so it is crucial to inform the healthcare provider about all the medications, vitamins, and supplements being taken. Drug interactions can affect the effectiveness of prednisone or increase the risk of side effects.
Conclusion: Prednisone is a powerful medication that is commonly used to treat various medical conditions. It is crucial to understand its usage, potential side effects, and drug interactions to ensure safe and effective treatment. If you have any concerns or questions about prednisone, it is advisable to consult with a healthcare provider.
Possible Side Effects
1. Increased Risk of Atrial Fibrillation
Taking prednisone may increase the risk of developing atrial fibrillation, a condition characterized by irregular heart rhythm. Research suggests that corticosteroids, like prednisone, can disrupt the normal electrical signals in the heart, leading to the development of atrial fibrillation. It is important to monitor heart health closely while taking prednisone and seek medical attention if any unusual symptoms, such as rapid or irregular heartbeat, occur.
2. Fluid Retention and Swelling
Prednisone can cause fluid retention and swelling in the body, particularly in the face, hands, and feet. This occurs due to the medication's ability to alter the body's fluid balance and sodium levels. It is important to monitor weight and keep an eye out for any noticeable changes in the body's appearance. If significant swelling or weight gain occurs, it is important to consult a healthcare professional, as this may indicate a need for a change in dosage or medication adjustment.
3. Increased Blood Pressure
Prednisone use has been associated with an increase in blood pressure. The medication can cause the body to retain water and sodium, leading to an increase in blood volume and subsequent rise in blood pressure. Individuals taking prednisone should have regular blood pressure monitoring and consult with their healthcare provider if there are any significant changes in blood pressure readings.
4. Mood and Behavioral Changes
Some individuals may experience mood and behavioral changes while taking prednisone. This can include feelings of irritability, anxiety, and even depression. These changes may be more pronounced for individuals who have a history of mental health disorders. It is important to discuss any concerning emotional or behavioral changes with a healthcare provider, as they may be able to adjust the medication or provide additional support.
5. Impaired Wound Healing
Prednisone can impair the body's natural healing process, making it more difficult for wounds to heal. It can delay the formation of new blood vessels and decrease the production of collagen, which are essential for wound healing. Individuals taking prednisone should take extra care to clean and care for wounds, and consult a healthcare professional if there are any concerns regarding wound healing.
6. Increased Risk of Infections
Prednisone can weaken the immune system, making individuals more susceptible to infections. It can suppress the body's natural defense mechanisms, such as white blood cell production, leaving the body vulnerable to bacterial and viral infections. It is important to take precautions to avoid exposure to infectious agents while taking prednisone and notify a healthcare provider if there are any signs of infection, such as fever, cough, or persistent sore throat.
Connection Between Prednisone and Atrial Fibrillation
Atrial fibrillation, a condition that causes irregular and rapid heartbeats, is a common cardiovascular disorder that affects millions of people worldwide. Research has shown that there may be a connection between the use of prednisone, a commonly prescribed corticosteroid, and the development of atrial fibrillation.
Several studies have found an association between prednisone use and an increased risk of developing atrial fibrillation. One study published in the Journal of the American College of Cardiology found that patients taking prednisone were almost twice as likely to develop atrial fibrillation compared to those not taking the drug.
The exact mechanism behind this connection is not well understood, but it is thought that prednisone may have an impact on the electrical properties of the heart, leading to the development of atrial fibrillation. Prednisone is known to have various effects on the immune system and inflammation, which may contribute to the development of cardiovascular complications.
It is important for healthcare providers to be aware of this potential link and carefully monitor patients who are prescribed prednisone, particularly those with pre-existing cardiovascular conditions. Patients should also be informed about the potential risks and benefits of taking prednisone and discuss alternative treatment options with their healthcare provider.
More research is needed to fully understand the connection between prednisone and atrial fibrillation and to determine the underlying mechanisms. In the meantime, individuals taking prednisone should be vigilant about any changes in their heart rhythm and seek medical attention if they experience symptoms of atrial fibrillation.
Studies and Research
The relationship between prednisone and atrial fibrillation has been the subject of several studies and research. Various research studies have investigated the potential link between prednisone use and the development or exacerbation of atrial fibrillation, a common heart rhythm disorder.
A study published in the Journal of Clinical Pharmacology examined the effects of prednisone on heart rhythm in a cohort of patients. The study found that prednisone use was associated with an increased risk of atrial fibrillation, particularly in patients with pre-existing heart conditions or risk factors for cardiovascular disease.
Another study published in the American Journal of Cardiology explored the relationship between prednisone use and the incidence of atrial fibrillation. The study analyzed a large database of patients and found that the use of prednisone was associated with a higher risk of developing atrial fibrillation, independent of other known risk factors.
Moreover, a systematic review and meta-analysis published in the European Heart Journal evaluated the available evidence on the association between glucocorticoid use, including prednisone, and atrial fibrillation. The analysis of multiple studies indicated that glucocorticoid use was significantly associated with an increased risk of atrial fibrillation.
Overall, these studies and research suggest that there is a potential link between prednisone use and the development or exacerbation of atrial fibrillation. However, it is important to note that individual responses to prednisone may vary, and further research is needed to fully understand the underlying mechanisms and potential interactions with other cardiovascular risk factors.
Managing Atrial Fibrillation while on Prednisone
1. Regular Monitoring
If you are taking Prednisone and have been diagnosed with atrial fibrillation (AF), it is important to regularly monitor your heart rhythm. This can be done through regular electrocardiogram (ECG) tests, which can detect any abnormal heart rhythms.
2. Medication Adjustments
It is crucial to work closely with your healthcare provider to manage your AF while on Prednisone. They may need to adjust your medication to ensure your heart rate and rhythm are controlled. This may involve adjusting the dosage or adding additional medications to manage your AF effectively.
3. Lifestyle Modification
Managing AF while on Prednisone also involves making lifestyle modifications. This may include adopting a heart-healthy diet, maintaining a healthy weight, avoiding excessive alcohol consumption, quitting smoking, and managing stress levels. These lifestyle changes can help reduce the risk of AF episodes.
4. Managing Side Effects
While taking Prednisone, be aware of any potential side effects that may worsen your AF symptoms. Common side effects include increased heart rate and fluid retention. If you experience any worsening of symptoms or side effects, inform your healthcare provider immediately.
5. Communication with Healthcare Provider
Regular communication with your healthcare provider is essential for managing AF while on Prednisone. It is important to keep them updated on any changes in your symptoms or medication side effects. They can provide guidance and make necessary adjustments to your treatment plan.
Remember, everyone's experience with AF while on Prednisone may vary. It is crucial to work closely with your healthcare provider to develop a personalized management plan that suits your specific needs and medical history.
Follow us on Twitter @Pharmaceuticals #Pharmacy
Subscribe on YouTube @PharmaceuticalsYouTube




Be the first to comment on "Prednisone cause afib"