Prednisone cause hives
When it comes to treating various conditions, prednisone is a commonly prescribed medication. However, while it can effectively alleviate symptoms and bring relief to patients, research has shown that it may also be connected to the occurrence of hives, a common allergic skin reaction. Understanding the link between prednisone and hives is crucial for both patients and healthcare professionals, as it can help identify potential side effects and provide appropriate management strategies.
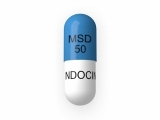
Prednisone is a corticosteroid medication that is often prescribed for its powerful anti-inflammatory properties. It is commonly used to treat conditions such as asthma, allergies, rheumatoid arthritis, and skin disorders. While prednisone can effectively suppress the immune system and reduce inflammation, it also has the potential to trigger allergic reactions in some individuals.
Hives, also known as urticaria, are itchy, raised welts on the skin that can appear suddenly and disappear within hours or days. They are commonly caused by allergic reactions to certain foods, medications, insect bites, or other allergens. When it comes to prednisone, studies have suggested that it can sometimes cause hives as a side effect, although the exact mechanisms behind this connection are still not fully understood.
If a patient experiences hives while taking prednisone, it is important to consult a healthcare professional for proper evaluation and management. In some cases, the medication may need to be adjusted or discontinued, and alternative treatment options may be explored. Identifying the connection between prednisone and hives can help ensure the safety and well-being of patients, enabling them to manage their conditions effectively and avoid potential allergic reactions.
In conclusion, prednisone is a commonly prescribed medication with a known link to hives, a common allergic skin reaction. While it can effectively treat various conditions, prednisone may trigger allergic reactions in some individuals, leading to the appearance of hives. Understanding this connection is vital for patients and healthcare professionals, as it can guide treatment decisions and ensure appropriate management strategies. If you are taking prednisone and notice the onset of hives, it is important to seek medical attention to address the issue and explore alternative treatment options if necessary.
Prednisone and its Connection to Hives
Hives, also known as urticaria, are itchy red welts that appear on the skin. They can be triggered by various factors, including allergies, infections, stress, and medications. Prednisone, a commonly prescribed corticosteroid medication, has been linked to the development of hives in some individuals.
How Prednisone Works:
Prednisone works by reducing inflammation in the body. It is commonly used to treat a wide range of conditions, including allergies, asthma, autoimmune diseases, and inflammatory conditions. However, in some cases, prednisone itself can cause allergic reactions, which may include the development of hives.
The Link Between Prednisone and Hives:
While prednisone is not a known common trigger for hives, there have been reports of individuals developing hives after taking the medication. These hives may appear shortly after starting the medication or even after prolonged use. The exact mechanism behind this connection is not fully understood, but it is believed that the immune system may be involved in the development of hives in response to prednisone.
Symptoms and Treatment:
If you develop hives while taking prednisone, it is important to inform your healthcare provider. They will evaluate your symptoms and determine the best course of action. In some cases, they may recommend adjusting the dosage of prednisone or switching to an alternative medication. Antihistamines may also be prescribed to relieve itching and reduce the severity of hives. Additionally, it is important to avoid known triggers and maintain good skin hygiene to help manage the symptoms of hives.
Conclusion:
While prednisone can be an effective medication for many conditions, it is important to be aware of the potential link to hives. If you experience hives while taking prednisone, consult your healthcare provider for proper evaluation and management. They will be able to determine the most appropriate course of action to address your symptoms and ensure your overall wellbeing.
Understanding Allergic Reactions
Allergic reactions occur when the immune system identifies certain substances, known as allergens, as harmful and reacts to them. These reactions can manifest in various ways, such as hives, sneezing, itching, or even life-threatening symptoms like anaphylaxis. The body's immune response to allergens involves the release of antibodies, specifically immunoglobulin E (IgE), which trigger the release of histamine and other chemicals.
Allergic reactions can be caused by a wide range of allergens, including certain foods, medications, insect bites, and environmental factors such as pollen or dust mites. The severity of the reaction can vary from person to person, with some individuals experiencing mild symptoms while others may have more severe or even life-threatening reactions.
Types of Allergic Reactions:
- Hives: Hives, also known as urticaria, are a common allergic reaction characterized by itchy, raised welts on the skin. These hives may vary in size and shape and can appear in clusters or as individual bumps. They can be triggered by a variety of factors, including certain medications like prednisone.
- Allergic rhinitis: Also known as hay fever, allergic rhinitis is characterized by symptoms such as sneezing, nasal congestion, runny nose, and itching of the eyes, nose, and throat. It is commonly triggered by allergens like pollen, dust mites, pet dander, or mold.
- Anaphylaxis: Anaphylaxis is a severe allergic reaction that can be life-threatening. It typically involves a rapid onset of symptoms, such as difficulty breathing, swelling of the face and throat, hives, dizziness, and a drop in blood pressure. Anaphylaxis requires immediate medical attention.
It is essential to identify the specific allergen causing the reaction in order to effectively manage and prevent future allergic episodes. Allergy testing, either through skin prick tests or blood tests, can help determine the specific allergens that trigger a person's immune response. Once identified, allergens can be avoided, and appropriate treatment options, such as antihistamines or epinephrine auto-injectors, can be prescribed to manage allergic reactions.
Exploring the Link Between Prednisone and Hives
Prednisone and its Role in Allergic Reactions
Prednisone is a medication that belongs to a class of drugs known as corticosteroids. It is commonly prescribed to treat various medical conditions, including allergies. However, it is important to note that prednisone itself can also be a trigger for allergic reactions, such as hives.
Hives: An Overview
Hives, also known as urticaria, are a common allergic reaction characterized by red, itchy welts that appear on the skin. They can be caused by a variety of factors, including certain foods, medications, and environmental triggers.
The Connection: When it comes to the link between prednisone and hives, research suggests that while prednisone is commonly used to treat allergic reactions, it can paradoxically also cause hives as a side effect in some individuals.
Possible Mechanisms
The exact mechanism by which prednisone triggers hives is still not fully understood. However, it is believed that prednisone can alter the immune system, leading to an overactive response that manifests as hives in certain individuals.
It is important to note that not everyone who takes prednisone will experience hives as a side effect. The occurrence of hives can vary depending on individual factors, such as the dose of prednisone, duration of treatment, and an individual's underlying susceptibility to allergic reactions.
Managing Hives While Taking Prednisone
If you develop hives while taking prednisone, it is important to inform your healthcare provider. They may recommend adjusting the dosage of prednisone or prescribing additional medications to help alleviate the symptoms of hives.
- Antihistamines: Antihistamines are commonly prescribed to help relieve the itching and redness associated with hives.
- Topical Treatments: In some cases, your healthcare provider may recommend using topical creams or ointments to reduce inflammation and soothe the affected areas of skin.
- Identifying Triggers: Keeping a record of your symptoms and potential triggers can help identify the underlying cause of hives and avoid future episodes.
Remember, it is important to consult with your healthcare provider before making any changes to your medication regimen or treatment plan.
Treatment Options for Prednisone-Induced Hives
1. Topical Treatments
Topical treatments can be used to relieve the itchiness and inflammation associated with prednisone-induced hives. These may include creams, gels, or ointments containing corticosteroids, such as hydrocortisone. Applying these topically can help reduce the redness and swelling, providing immediate relief.
Additionally, non-steroidal creams or lotions, such as calamine lotion or aloe vera gel, can be applied to soothe the skin and alleviate discomfort caused by hives.
2. Antihistamines
Antihistamines are commonly used to treat allergic reactions, including hives. These medications work by blocking the release of histamine, a chemical responsible for triggering itching, swelling, and redness. Over-the-counter antihistamines like cetirizine, loratadine, or diphenhydramine can be effective in relieving the symptoms of prednisone-induced hives.
If over-the-counter antihistamines do not provide sufficient relief, a healthcare professional may prescribe stronger antihistamines, such as fexofenadine or levocetirizine.
3. Steroid Tapering
In some cases, prednisone-induced hives may require the gradual reduction or tapering of the prednisone dosage. This approach helps to prevent abrupt withdrawal, which can trigger a rebound effect and worsen the hives. It is important to consult with a healthcare professional to determine the appropriate tapering schedule based on individual circumstances.
4. Immunosuppressants
In severe cases of prednisone-induced hives that do not respond to other treatments, a healthcare professional may consider prescribing immunosuppressant medications. These medications work by suppressing the immune system to reduce the allergic response causing the hives. Immunosuppressants may be used for short-term management of hives until the underlying cause, such as the discontinuation of prednisone, is resolved.
5. Prevention and Management
Prevention and management strategies play an important role in reducing the occurrence and severity of prednisone-induced hives. It is essential to avoid any known triggers or allergens that may exacerbate the condition. Maintaining good skin hygiene, using hypoallergenic products, and avoiding excessive heat or sweating can also help prevent hives. If hives do occur, keeping the affected area cool and moisturized can provide some relief.
If symptoms worsen or persist despite treatment, it is crucial to seek medical attention for further evaluation and guidance.
Seeking Medical Advice
If you are experiencing hives while taking prednisone, it is important to seek medical advice. Your healthcare provider is the best person to assess your situation and determine the appropriate course of action. They will be able to evaluate your symptoms, review your medical history, and make an informed decision about the next steps.
1. Consult with your doctor: Schedule an appointment with your doctor to discuss your symptoms and any concerns you may have. Your doctor will be able to assess your condition and determine if prednisone is the cause of your hives or if there may be another underlying cause.
2. Provide necessary information: During your appointment, be prepared to provide your doctor with detailed information about your symptoms and the timeline of when they first appeared. Inform them if you have recently started or stopped taking any medications, including prednisone, as this may be a potential trigger for the hives.
3. Undergo testing if necessary: Depending on your symptoms and medical history, your doctor may recommend further testing to confirm the cause of your hives. This could include blood tests or allergy testing to identify any potential allergens that may be triggering the hives.
4. Discuss alternative treatments: If prednisone is found to be the cause of your hives, your doctor may recommend alternative treatments. They may prescribe a different medication or adjust the dosage of prednisone to alleviate your symptoms. It is important to carefully follow your doctor's instructions and report any changes or side effects.
5. Seek immediate medical attention for severe symptoms: If you experience severe symptoms such as difficulty breathing, swelling of the face or throat, or a rapid onset of hives, seek immediate medical attention. These symptoms may indicate a severe allergic reaction, and prompt medical intervention is vital.
Remember, it is always important to seek medical advice when experiencing any unusual symptoms. Your doctor is there to help you navigate your health concerns and provide the best possible care.
Follow us on Twitter @Pharmaceuticals #Pharmacy
Subscribe on YouTube @PharmaceuticalsYouTube



Be the first to comment on "Prednisone cause hives"